Psyllium Husk for Diverticulitis | Safe Laxative Use & Management Guide – 2026
Managing diverticulitis requires careful attention to fiber intake, and understanding how to use psyllium husk for diverticulitis can make the difference between comfortable management and painful flare-ups. Unlike harsh chemical laxatives, psyllium husk as a laxative works gently with your body’s natural processes to promote regularity without irritation or dependency.
Diverticulitis affects millions globally, creating painful inflammation in small pouches (diverticula) that form in the colon wall. The relationship between fiber, laxatives, and diverticular disease is nuanced – timing matters tremendously. During acute flare-ups, high fiber can worsen symptoms, but between episodes, appropriate fiber intake actually prevents future problems.
This creates confusion. Should you use psyllium husk for diverticulitis or avoid it? When is it safe? How does psyllium husk as a laxative differ from stimulant laxatives? What dosing prevents complications?
This comprehensive guide answers these critical questions with evidence-based protocols. You’ll learn when psyllium is beneficial versus harmful for diverticulitis, how it compares to other laxative options, proper dosing during different disease phases, and strategies to prevent diverticulitis recurrence through intelligent fiber management. Whether you’re newly diagnosed, managing chronic diverticular disease, or seeking a gentle laxative alternative, this guide provides the clarity you need for safe, effective psyllium use.
Understanding Diverticulitis and Fiber’s Role
Before exploring psyllium’s specific applications, let’s clarify what diverticulitis is and how fiber affects it.
What Are Diverticula and Diverticulitis?
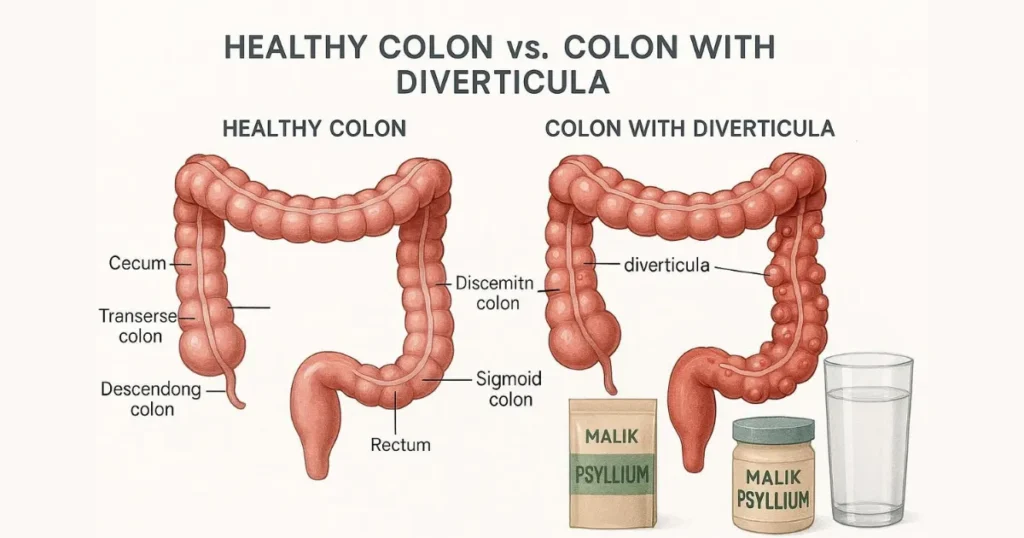
Diverticula are small, bulging pouches that form in the lining of your digestive system, most commonly in the lower colon. When you have these pouches without symptoms, it’s called diverticulosis. When they become inflamed or infected, that’s diverticulitis.
The progression typically follows this pattern:
Diverticulosis:
Pouches form due to weak spots in the colon wall. Often symptom-free. Extremely common after age 60 – about 50% of people over 60 have diverticula.
Diverticular disease:
Pouches cause occasional discomfort, bloating, or irregular bowel movements but aren’t acutely inflamed.
Diverticulitis:
Active inflammation or infection in the pouches, causing severe abdominal pain, fever, nausea, and changes in bowel habits. This requires medical treatment.
The Fiber Paradox in Diverticular Disease
Here’s what confuses people: fiber’s role changes depending on the disease phase.
During acute diverticulitis:
Low-fiber or even liquid diets are recommended. Fiber can irritate inflamed diverticula, worsening pain and potentially causing complications. This is NOT the time to increase fiber intake.
During remission (between flare-ups):
High-fiber diets reduce diverticulitis recurrence by 40-50% according to research. Fiber prevents the straining and increased colon pressure that leads to pouch formation and inflammation.
This timing is critical. Using psyllium husk for diverticulitis appropriately means knowing which phase you’re in.
Psyllium Husk as a Laxative: How It Works
Understanding psyllium’s laxative mechanism helps explain why it’s beneficial for diverticular disease management – when used correctly.
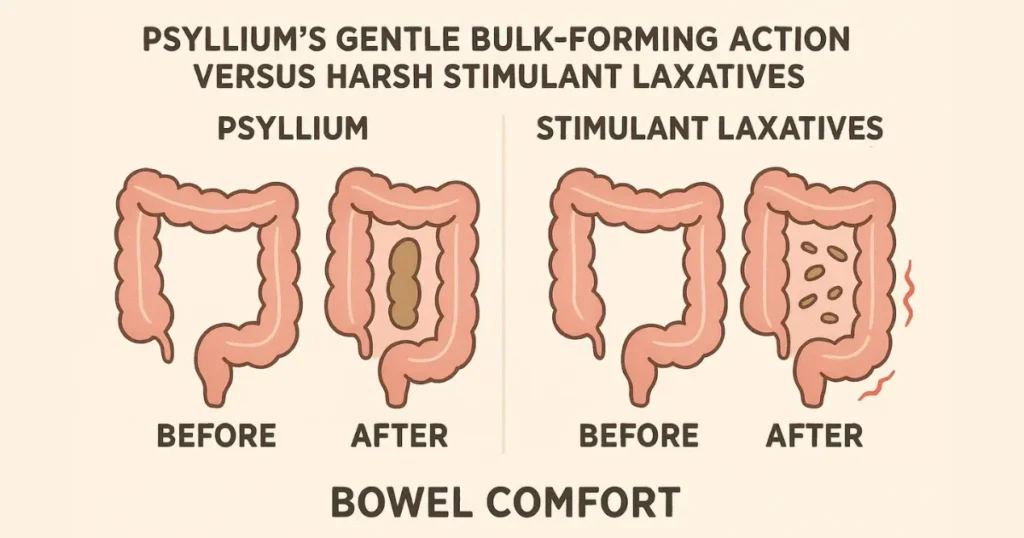
Bulk-Forming Laxative Classification
Psyllium falls into the “bulk-forming laxative” category, distinctly different from stimulant, osmotic, or lubricant laxatives.
How psyllium works:
- Absorbs water in the intestines (10-20x its weight).
- Forms a gel-like mass that softens stool.
- Increases stool bulk, triggering natural peristalsis.
- Doesn’t chemically stimulate the bowel.
- Works gently over 12-72 hours.
This gentle mechanism makes psyllium husk as a laxative ideal for chronic constipation management without the harsh effects of stimulant laxatives like senna or bisacodyl.
Advantages Over Other Laxatives.
Compared to stimulant laxatives:
- No dependency risk.
- No bowel cramping or urgency.
- Maintains natural bowel function.
- Safe for long-term use.
- Doesn’t deplete electrolytes.
Compared to osmotic laxatives:
- Less bloating and gas (when properly introduced).
- More predictable effects.
- Better for daily maintenance.
- Doesn’t draw excessive water into bowels.
Compared to stool softeners:
- More effective for constipation.
- Addresses root causes, not just symptoms.
- Provides additional health benefits (cholesterol, blood sugar).
For diverticular disease patients who often struggle with chronic constipation, psyllium offers sustainable relief without the complications of harsher laxatives.
The Prebiotic Benefit.
Unlike synthetic laxatives, psyllium feeds beneficial gut bacteria. This prebiotic effect supports overall colon health, potentially reducing inflammation that contributes to diverticulitis flare-ups. The fermentation of psyllium fiber produces short-chain fatty acids that nourish colon cells and support the intestinal barrier.
Using Psyllium Husk for Diverticulitis: Phase-Based Protocols.
Safe psyllium husk diverticulitis use in diverticular disease requires understanding which phase you’re in and adjusting accordingly.
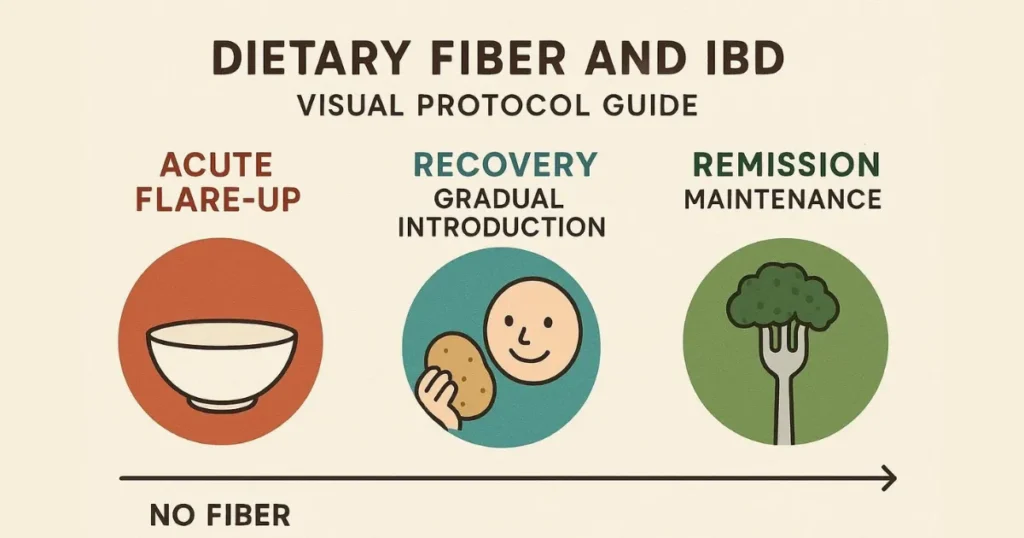
During Acute Diverticulitis (Active Flare-Up).
DO NOT use psyllium during active inflammation. This is critical.
Symptoms of acute diverticulitis include:
- Severe abdominal pain (usually lower left side).
- Fever.
- Nausea or vomiting.
- Marked change in bowel habits.
- Tenderness when touching the abdomen.
During flare-ups, your gastroenterologist will typically recommend:
- Clear liquid diet initially.
- Gradual progression to low-fiber foods.
- Antibiotics if bacterial infection is present.
- Complete bowel rest in severe cases.
Introducing psyllium or any high-fiber foods during this phase can worsen inflammation, increase pain, and potentially lead to complications like perforation or abscess formation.
During Recovery (Transitioning from Flare-Up).
Once acute symptoms resolve – typically 7-14 days after treatment begins – you can gradually reintroduce fiber.
Week 1 post-flare:
Continue low-fiber diet. No psyllium yet.
Week 2 post-flare:
If symptom-free, begin introducing soft, easily digestible fiber from cooked vegetables and refined grains.
Week 3-4 post-flare:
Start psyllium at very low doses – just ⅛ to 1/4 teaspoon daily. Monitor for any pain or discomfort.
Week 5+ post-flare:
Gradually increase psyllium to maintenance doses (1-2 teaspoons daily) if well-tolerated.
This conservative approach prevents triggering another flare-up during the vulnerable recovery period.
During Remission (Preventive Maintenance).
When you’re symptom-free between flare-ups, psyllium becomes your ally for preventing recurrence.
Maintenance protocol:
- 1-2 teaspoons of psyllium husk daily.
- Split into 1-2 doses.
- Taken with at least 8-10 ounces of water per dose.
- Consistent timing (same time daily).
- Combined with a high-fiber diet (25-35g total daily fiber).
Research shows that maintaining 25-35 grams of daily fiber reduces diverticulitis recurrence significantly. Psyllium provides 5-10 grams of this target, making the remainder easier to achieve through diet.
Psyllium Dosing Protocols for Diverticular Disease.
Proper dosing prevents complications while maximizing the benefits of psyllium husk for diverticulitis.

Starting Protocol for Diverticulosis (No Active Inflammation).
If you have diverticula but no current inflammation:
- Week 1: 1/4 teaspoon once daily with 8-10 oz water.
- Week 2: 1/2 teaspoon once daily.
- Week 3: 3/4 teaspoon once daily or 1/2 teaspoon twice daily.
- Week 4+: 1-2 teaspoons daily (split into 1-2 doses).
This gradual increase allows your digestive system to adapt without triggering symptoms.
Maintenance Dosing.
Once established, most diverticular disease patients do well with:
- Conservative approach: 1 teaspoon (5g) daily.
- Standard approach: 1-2 teaspoons (5-10g) daily.
- Aggressive prevention: 2-3 teaspoons (10-15g) daily.
Work with your gastroenterologist to determine your optimal maintenance dose based on symptom history, severity, and recurrence frequency.
Hydration Requirements.
Inadequate water with psyllium can worsen constipation and increase colon pressure – exactly what diverticular disease patients need to avoid.
Minimum requirements:
- 8-10 oz water mixed with each psyllium dose.
- Another 8 oz of water, 30 minutes later.
- 10-12 glasses total throughout the day.
Proper hydration is non-negotiable for safe psyllium use in diverticulitis management.
Comparing Psyllium to Other Laxative Options for Diverticulitis.
Let me share how psyllium stacks up against other common laxatives for diverticular disease management.
Psyllium vs. Stimulant Laxatives (Senna, Bisacodyl).
| Aspect | Psyllium | Stimulant Laxatives |
| Mechanism | Bulk-forming, natural | Chemical bowel stimulation |
| Safety for diverticulitis | Safe during remission | Can increase colon pressure |
| Long-term use | Recommended | Causes dependency |
| Side effects | Minimal when dosed properly | Cramping, urgency, electrolyte loss |
| Flare-up prevention | Yes—reduces recurrence | No preventive benefit |
Stimulant laxatives should be avoided or used only occasionally by diverticulitis patients. They increase colon pressure and spasms, potentially triggering flare-ups.
Psyllium vs. MiraLAX (Polyethylene Glycol).
MiraLAX is an osmotic laxative commonly prescribed for constipation.
Advantages of MiraLAX:
- Very gentle, minimal bloating.
- Safe during diverticulitis flare-ups (unlike fiber).
- Predictable results.
- No fermentation or gas production.
Advantages of psyllium:
- Provides actual fiber (cardiovascular, metabolic benefits).
- Feeds beneficial bacteria.
- More natural option.
- Costs less long-term.
- Prevents diverticulitis recurrence.
Many gastroenterologists recommend MiraLAX during and immediately after flare-ups, then transitioning to psyllium for long-term maintenance.
Psyllium vs. Wheat Bran and Insoluble Fiber.
Some doctors recommend wheat bran for diverticular disease, but psyllium offers distinct advantages:
Why psyllium is often better:
- Soluble fiber is gentler on inflamed diverticula.
- Less gas and bloating than wheat bran.
- Better studied for diverticulitis prevention.
- Easier to dose consistently.
- Superior stool softening (reduces straining).
Insoluble fiber, like wheat bran, can be too rough for sensitive colons, especially soon after flare-ups. Psyllium’s soluble fiber provides gentler bulk without mechanical irritation.
Benefits of Psyllium Beyond Laxative Effects.
Using psyllium husk for diverticulitis provides benefits beyond simple bowel regulation.
Reduces Straining and Colon Pressure.
Straining during bowel movements increases intra-colonic pressure, contributing to both diverticula formation and inflammation of existing pouches. Psyllium’s stool-softening effect eliminates straining, directly addressing one of diverticulitis’s root causes.
Supports Healthy Gut Microbiome.
The prebiotic fiber in psyllium feeds beneficial bacteria, supporting immune function and reducing systemic inflammation. A healthier microbiome may reduce the inflammatory response that turns diverticulosis into diverticulitis.
Regulates Bowel Transit Time.
Psyllium normalizes transit time – it helps both constipation and diarrhea. For diverticular disease patients who experience alternating bowel patterns, this regulatory effect provides consistent comfort.
Addresses Common Comorbidities.
Diverticular disease often coexists with:
- High cholesterol (psyllium reduces LDL by 5-10%).
- Diabetes or insulin resistance (psyllium improves blood sugar control).
- Obesity (psyllium supports weight management through satiety).
- Hypertension (modest blood pressure reduction with regular use).
These cardiovascular and metabolic benefits make psyllium particularly valuable for the demographic most affected by diverticular disease.
Safety Considerations and Contraindications.
While psyllium is generally safe, certain situations require extra caution or complete avoidance.
When to Avoid Psyllium Completely.
Never use psyllium if you have:
- Active diverticulitis with symptoms.
- Suspected bowel obstruction.
- Difficulty swallowing.
- Known psyllium allergy.
- Recent intestinal surgery (unless approved by surgeon).
- Severe diverticulitis with complications (abscess, perforation, fistula).
Warning Signs to Stop Immediately.
Discontinue psyllium and contact your doctor if you experience:
- New or worsening abdominal pain.
- Fever.
- Blood in stool.
- Severe bloating or distension.
- Inability to pass gas or stool.
- Nausea or vomiting.
These symptoms may indicate a diverticulitis flare-up or other complications requiring medical evaluation.
Medication Interactions.
Psyllium can affect medication absorption. Take psyllium 2-4 hours away from:
- Blood thinners (warfarin).
- Diabetes medications.
- Thyroid hormones.
- Heart medications.
This is particularly important for diverticulitis patients, who may be on multiple medications for related conditions.
Quality Matters: Choosing the Right Psyllium.
For diverticular disease management, psyllium quality significantly impacts results and tolerability.

Why Pakistani Psyllium Excels.
Pakistani psyllium, particularly from Sindh province, offers 95-99% purity – the highest available globally. This matters for diverticulitis patients because:
Higher purity means:
- More predictable fiber content and effects.
- Fewer impurities that could irritate sensitive colons.
- Reduced risk of contamination.
- More reliable dosing consistency.
At Malik Psyllium, our multi-stage processing ensures pharmaceutical-grade purity. For patients managing inflammatory bowel conditions, this quality difference isn’t a luxury – it’s essential for safe, predictable results.
Avoiding Low-Quality Products.
Cheap psyllium often contains:
- Seed particles that can lodge in diverticula.
- Processing residues that irritate the intestines.
- Inconsistent fiber content.
- Potential contaminants.
For diverticulitis patients, these impurities could potentially trigger inflammation or worsen symptoms. Premium quality psyllium is worth the modest additional cost.
Lifestyle Integration for Diverticulitis Management.
Psyllium works best as part of comprehensive diverticular disease management.

Combining Psyllium with Dietary Fiber.
Don’t rely solely on psyllium. Combine it with naturally fiber-rich foods:
Excellent sources:
- Cooked vegetables (avoid raw during sensitive periods).
- Fruits with edible skins (apples, pears).
- Whole grains (oatmeal, brown rice).
- Legumes (beans, lentils – introduce gradually).
Target 25-35 grams total daily fiber, with psyllium providing 5-10 grams of this goal.
Hydration Strategy.
Beyond the water consumed with psyllium, maintain excellent overall hydration:
- 8-10 glasses of water daily minimum.
- Herbal teas count toward fluid intake.
- Limit caffeine and alcohol (both dehydrating).
- Increase fluids during hot weather or exercise.
Dehydration contributes to constipation and increases diverticulitis risk.
Physical Activity.
Regular movement supports healthy bowel function and reduces diverticulitis recurrence risk. Aim for:
- 30 minutes of moderate activity daily.
- Walking after meals aids digestion.
- Avoid heavy lifting or straining.
- Core exercises strengthen abdominal muscles (consult a doctor first).
Stress Management.
Stress affects gut motility and inflammation. Incorporate:
- Meditation or mindfulness practices.
- Adequate sleep (7-9 hours nightly).
- Stress-reduction techniques that work for you.
- Regular relaxation time.
Common Myths about Psyllium and Diverticulitis.
Let me clarify some widespread misconceptions.
Myth 1: “Seeds and Nuts Cause Diverticulitis, So Avoid Psyllium Seeds”.
Outdated advice suggested avoiding seeds and nuts, but research has debunked this. Psyllium husk (the fiber coating) is what’s used – not the seeds themselves. Quality psyllium products contain no whole seeds.
Myth 2: “If You Have Diverticula, You Can Never Use Fiber Supplements”.
False. While fiber is contraindicated during acute inflammation, it’s actually recommended for prevention between flare-ups. The key is timing and gradual introduction.
Myth 3: “Psyllium Will Make Diverticulitis Worse”.
Only if used during active inflammation. During remission, psyllium reduces recurrence risk by preventing constipation and straining that trigger flare-ups.
Myth 4: “Natural Laxatives Like Psyllium Are Weaker Than Prescription Options”.
For chronic management, bulk-forming laxatives like psyllium are often more effective and safer than stimulant laxatives. They address causes rather than just symptoms.
Working with Your Healthcare Team.
Managing diverticulitis with psyllium requires medical oversight.
When to Consult Your Doctor.
Discuss psyllium with your gastroenterologist if you:
- Have been recently diagnosed with diverticulosis or diverticulitis.
- Experienced a diverticulitis flare-up in the past 3 months.
- Take multiple medications.
- Have other digestive conditions (IBS, IBD, etc).
- Experience any unusual symptoms after starting psyllium.
Monitoring for Success.
Track these indicators to assess whether psyllium is helping:
Positive signs:
Regular, comfortable bowel movements.
- Reduced straining.
- No diverticulitis flare-ups.
- Less abdominal discomfort.
- Improved energy and wellbeing.
Concerning signs:
- Increased pain or discomfort.
- New symptoms.
- Worsening constipation despite psyllium.
- Frequent bloating or gas.
Regular communication with your healthcare provider ensures optimal management.
Real-World Success with Psyllium for Diverticular Disease.
Over the years, I’ve seen countless individuals successfully manage diverticular disease with appropriate psyllium use. The pattern is consistent: those who follow gradual introduction protocols, maintain excellent hydration, and use psyllium consistently between flare-ups experience significantly fewer recurrences than those who don’t.
One key observation: patience matters. People who rush the introduction process or use psyllium inconsistently don’t get the protective benefits. But those who commit to daily use as part of their wellness routine – much like taking daily vitamins – see remarkable improvement in symptom frequency and severity.
The quality factor is equally important. Premium Pakistani psyllium from sources like Malik Psyllium provides the consistency and purity that sensitive digestive systems need. Lower-grade products can create unpredictable results that undermine confidence in fiber supplementation.
Is psyllium husk safe for diverticulitis?
Psyllium husk for diverticulitis is safe and beneficial during remission but must be avoided during acute flare-ups. Start gradually once inflammation resolves, and work with your gastroenterologist for personalized timing and dosing guidance.
How does psyllium husk work as a laxative?
Psyllium husk as a laxative works by absorbing water and forming a gel that softens stool, increases bulk, and triggers natural bowel movements. Unlike stimulant laxatives, it’s gentle, non-habit-forming, and safe for long-term use.
When should I start using psyllium after a diverticulitis flare-up?
Wait until acute symptoms completely resolve (typically 2-3 weeks), then start with very small doses – ⅛ to 1/4 teaspoon daily – gradually increasing over 4-6 weeks. Always follow your doctor’s specific recommendations for your case.
Can psyllium prevent diverticulitis recurrence?
Yes, research shows that adequate fiber intake (including psyllium) reduces diverticulitis recurrence by 40-50%. Consistent daily use during remission helps prevent the constipation and straining that trigger flare-ups.
How much water do I need with psyllium for diverticulitis?
Drink at least 8-10 ounces with each psyllium dose, followed by another 8 ounces within 30 minutes. Aim for 10-12 glasses total daily. Inadequate hydration can worsen constipation and increase diverticulitis risk.
Is psyllium better than other laxatives for diverticular disease?
For long-term management, psyllium is superior to stimulant laxatives (which can increase colon pressure) and offers more benefits than simple stool softeners. It’s the preferred fiber supplement for diverticulitis prevention.
What’s the difference between psyllium and MiraLAX for diverticulitis?
MiraLAX is safer during flare-ups, while psyllium is better for long-term prevention. Many doctors recommend MiraLAX during inflammation, then transitioning to psyllium for maintenance once symptoms resolve.
Can I use psyllium husk if I have both diverticulitis and IBS?
Possibly, but this requires careful medical supervision. Introduce psyllium very gradually and monitor symptoms closely. Some IBS patients tolerate psyllium well; others find it increases bloating. Work with your gastroenterologist to find the right approach.
Conclusion.
Understanding how to safely use psyllium husk for diverticulitis can transform disease management from reactive crisis control to proactive prevention. The key is respecting the disease’s phases – avoiding fiber during acute inflammation while embracing it during remission as your primary prevention strategy.
Psyllium husk as a laxative offers diverticular disease patients a gentle, sustainable solution for the chronic constipation that often triggers flare-ups. Unlike stimulant laxatives that create dependency and increase colon pressure, psyllium works with your body’s natural processes to maintain comfortable, regular elimination without harmful side effects.
The protocol is straightforward but requires discipline: avoid psyllium completely during active diverticulitis, reintroduce it gradually during recovery, and maintain consistent daily use during remission. Combined with adequate hydration, a balanced fiber-rich diet, and healthy lifestyle habits, this approach reduces recurrence risk by 40-50% according to research.
Quality matters significantly for sensitive digestive systems managing inflammatory conditions. Pakistani psyllium from reputable sources like Malik Psyllium provides the pharmaceutical-grade purity that makes dosing predictable and results reliable. When managing diverticular disease, consistency and quality aren’t luxuries – they’re essential components of successful long-term management.
Work closely with your gastroenterologist, follow phase-appropriate protocols, maintain excellent hydration, and give psyllium time to demonstrate its protective benefits. Most patients who commit to this approach experience fewer, less severe flare-ups and enjoy significantly improved quality of life between episodes.
Malik Shabbir
Featured Blogs

Isabgol Ke Fayde – Psyllium Husk Ke Poori Science-Based Rahnumayi – 2026
Isabgol ke fayde jaanna aaj ke daur mein zyada zaroori

Isabgol Benefits in Hindi | Psyllium Husk Ke Fayde, Sahi Upyog Aur Savdhaniyan – 2026
Agar aap isabgol benefits in hindi mein samajhna chahte hain,
