Psyllium Husk and Medication Absorption | Essential Timing Guide for Safe Use – 2026

Understanding the relationship between psyllium husk and medication absorption is crucial for anyone taking daily prescriptions. Psyllium’s powerful fiber content – the same property that makes it so effective for digestive health – can interfere with how your body absorbs certain medications if timing isn’t managed properly.
This isn’t about avoiding psyllium. It’s about using it intelligently alongside your medications. The good news? With proper timing and format selection, you can safely enjoy psyllium’s benefits without compromising your treatment effectiveness. Whether you’re considering psyllium husk tablets, psyllium husk capsules, or traditional powder, understanding absorption dynamics is essential.
Many people don’t realize that the form of psyllium matters too. Psyllium husk tablets and capsules release fiber differently than powder, which affects both medication interactions and convenience. This guide covers everything you need to know: which medications are affected, optimal timing protocols, form selection, and practical strategies for integrating psyllium into your medication routine. Let’s explore how to maximize both your medication effectiveness and psyllium’s remarkable health benefits without compromise.
How Psyllium Husk Affects Medication Absorption
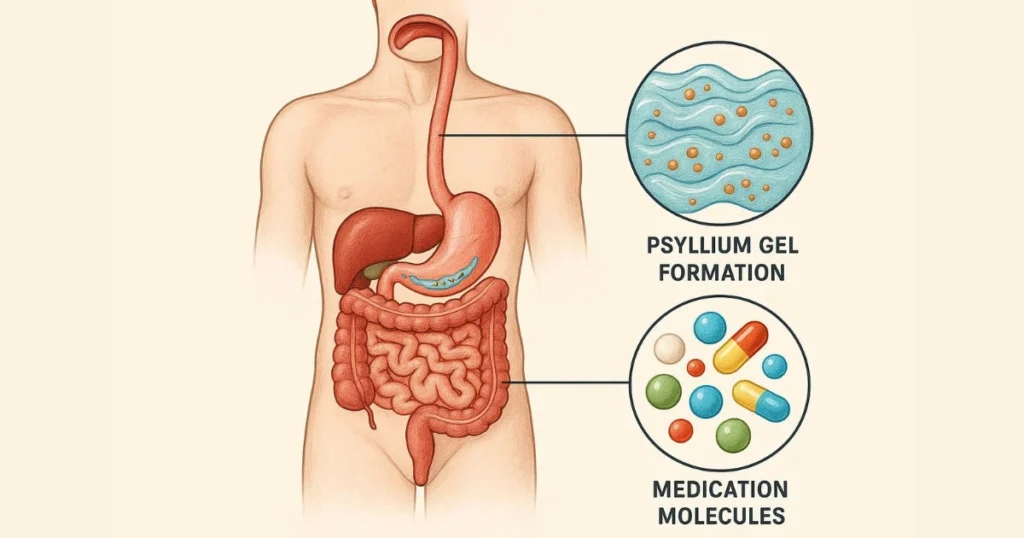
Psyllium husk contains approximately 70% soluble fiber that forms a viscous gel when mixed with liquid in your digestive system. This gel-forming property is precisely what makes psyllium so effective for digestive health – but it’s also why psyllium husk and medication absorption need careful consideration.
The Absorption Mechanism
When you take medications orally, they must be absorbed through your intestinal walls to enter your bloodstream. Psyllium’s gel creates a physical barrier that can:
Bind directly to medication molecules:
The gel traps drug particles, preventing them from reaching absorption sites.
Slow gastric emptying:
Psyllium keeps contents in your stomach longer, delaying medication release.
Coat intestinal walls:
The fiber layer reduces direct contact between medications and absorption surfaces.
Alter transit time:
Changing the movement through your digestive tract affects when and where absorption occurs.
These effects aren’t harmful in themselves – they simply mean less medication reaches your bloodstream, potentially making your treatment less effective. The solution isn’t avoiding psyllium but timing it correctly.
Why Timing Matters So Much
Most medications are designed to reach peak blood levels within 1-4 hours of ingestion. If psyllium interferes during this critical window, therapeutic levels may never be achieved. For medications with narrow therapeutic ranges – where small changes in blood levels significantly impact effectiveness – this becomes especially important.
Different psyllium forms also affect timing differently. Psyllium husk tablets and psyllium husk capsules dissolve more slowly than powder, creating extended interference windows that require adjusted timing protocols.
Medications Most Affected by Psyllium Husk
Not all medications interact equally with psyllium. Let me break down which drugs require the most careful attention to timing.
Critical Medications Requiring 4-Hour Separation
Thyroid medications (levothyroxine, Synthroid):
These have notoriously finicky absorption. Even small reductions in thyroid hormone levels cause symptoms. I always recommend taking thyroid medication on an empty stomach first thing in the morning, with psyllium reserved for later in the day – at least 4 hours apart.
Diabetes medications (metformin, glipizide, insulin):
Ironically, psyllium itself helps regulate blood sugar. However, it can reduce the absorption of oral diabetes drugs. The solution is careful timing and monitoring blood sugar levels when starting psyllium to adjust medication doses if needed.
Heart medications (digoxin, carvedilol):
These drugs have narrow therapeutic windows. Too little is ineffective; too much is toxic. Psyllium interference can push levels below effective ranges. Four-hour separation is essential, and periodic blood level monitoring is wise.
Blood thinners (warfarin):
While psyllium doesn’t directly interact with warfarin, it affects vitamin K absorption, which influences warfarin effectiveness. Consistency matters more than avoidance – use psyllium at the same time daily if you’re on warfarin, and monitor INR levels closely.
Medications Requiring 2-3 Hour Separation
Antibiotics (tetracycline, penicillin):
Fiber reduces antibiotic absorption, potentially undermining infection treatment. Take antibiotics well before or after psyllium doses.
Antidepressants (lithium, tricyclics):
These require consistent blood levels. Psyllium won’t cause immediate problems, but inconsistent timing may affect mood stability over time.
Seizure medications (carbamazepine, phenytoin):
Maintaining stable blood levels prevents breakthrough seizures. Separate psyllium by 2-3 hours from these medications.
Pain relievers (aspirin, NSAIDs):
Less critical than others, but separating by 1-2 hours optimizes absorption.
Medications Generally Safe with Psyllium
Topical medications:
No interaction since they’re not absorbed through the gut.
Injectable medications:
Bypass digestive absorption entirely.
Most vitamins and supplements:
May have reduced absorption, but typically not clinically significant (except fat-soluble vitamins with very high-dose psyllium).
Psyllium Husk Tablets vs. Capsules: Absorption Considerations
Format choice significantly impacts both convenience and medication interactions. Let me share what matters when choosing between psyllium husk tablets, psyllium husk capsules, and traditional powder.

Psyllium Husk Tablets
Tablets are compressed psyllium powder bound with minimal additives. They offer:
Pros:
- Precise, consistent dosing
- No preparation or mixing required
- Travel-friendly and discreet
- No taste or texture issues
- Slower fiber release may reduce gas for some users
Cons:
- Longer dissolution time (20-30 minutes).
- Extended medication interference window.
- Must drink substantial water with them.
- It may be harder to swallow for some people.
- Slightly more expensive per dose.
For medication timing, psyllium husk tablets require the most separation – ideally 3-4 hours from critical medications. Their slow dissolution means they continue releasing fiber for longer periods.
Psyllium Husk Capsules.
Capsules contain psyllium powder in gelatin or vegetarian shells. They provide:
Pros:
- Easy to swallow.
- No taste whatsoever.
- Convenient for people who dislike powder texture.
- Portable and mess-free.
- Quick to take.
Cons:
- Typically lower psyllium content per capsule (require 5-8 capsules per dose).
- More expensive than powder.
- Dissolution time varies by capsule type.
- Still requires substantial water intake.
- May cause reflux if not taken with enough liquid.
Psyllium husk capsules fall between tablets and powder for medication timing – typically requiring 2-3 hours of separation from critical medications.
Traditional Powder.
Loose psyllium powder remains the most economical and fastest-acting option:
Pros:
- Immediate fiber release when mixed with liquid.
- Shortest medication interference window.
- Most economical.
- Flexible dosing.
- Highest purity options available.
Cons:
- Requires mixing and preparation.
- Texture bothers some users.
- Less convenient for travel.
- Must be consumed immediately after mixing.
- Messier to handle.
For managing psyllium husk and medication absorption, powder offers the most control. You can time it precisely and know exactly when the fiber is active in your system.
Which Format for Medication Users?
- Choose powder if: You take multiple critical medications and need precise timing control.
- Choose capsules if: You take 1-2 medications that aren’t time-critical and value convenience.
- Choose tablets if: You need portability and your medications allow 3-4 hour separation windows.
Regardless of format, Pakistani psyllium offers superior purity – typically 95-99% – meaning more actual fiber per dose and fewer fillers that might complicate absorption issues.
Optimal Timing Protocols for Medication Users.
Let me share practical timing strategies that work in real life, not just in theory.
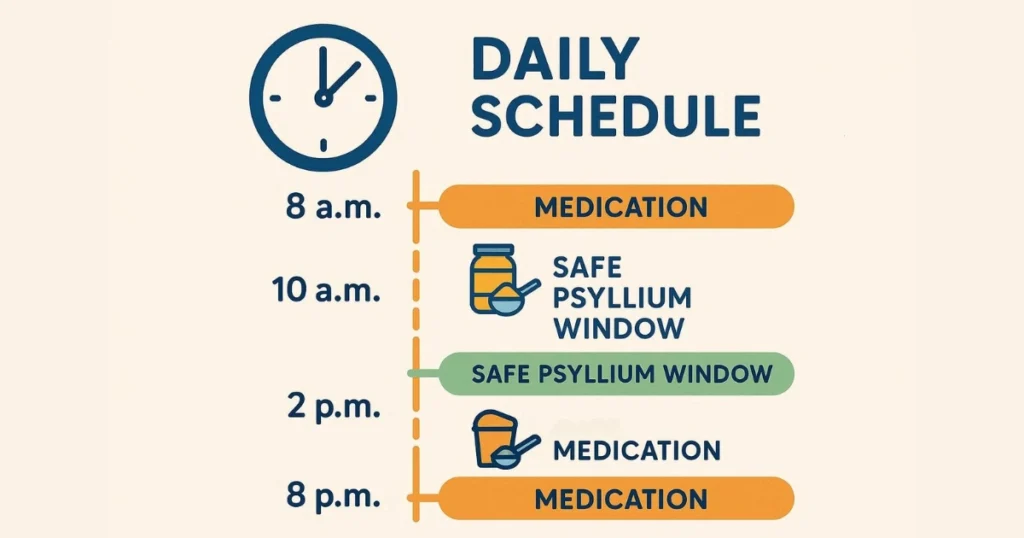
Morning Medication Schedule.
Many people take medications first thing in the morning. Here’s how to integrate psyllium:
- 6:00 AM: Take morning medications (thyroid, blood pressure, etc) with water on an empty stomach.
- 6:30 AM: Light breakfast.
- 10:00 AM: Take psyllium (powder, capsules, or tablets) with a full glass of water.
- 12:00 PM: Lunch and any midday medications.
This schedule ensures 4 hours between critical morning medications and psyllium, allowing complete absorption before fiber interference.
Evening Medication Schedule.
For evening medications like statins or acid reflux drugs:
- 6:00 PM: Dinner.
- 7:00 PM: Take psyllium with water.
- 11:00 PM: Evening medications before bed.
This provides 4 hours of separation while working with natural meal timing.
Multiple Daily Medication Schedule.
If you take medications throughout the day, split your psyllium dose:
- Morning: Half dose psyllium between breakfast and lunch medications.
- Evening: Half dose of psyllium between dinner and bedtime medications.
This maintains fiber benefits while creating multiple safe windows for medication absorption.
The “Bookmark” Method.
I call this the bookmark method: use medications as bookmarks in your day, with psyllium filling the gaps. Map out when you take each medication, then schedule psyllium in the longest gaps that provide at least 2-3 hours of separation.
Special Considerations for Different Health Conditions.
Diabetes Management.
Psyllium offers significant blood sugar benefits for diabetics, but managing psyllium husk and medication absorption requires extra attention. Monitor blood glucose when starting psyllium – your medication needs might decrease as psyllium improves sugar control. Work with your endocrinologist to adjust medications rather than stopping psyllium.
Thyroid Disorders.
Thyroid patients face particular challenges. Levothyroxine must be taken on an empty stomach, absorbed within 1-2 hours, and is notoriously affected by fiber. My recommendation: thyroid medication first thing in the morning, psyllium at lunch or dinner – never closer than 4 hours.
Cardiovascular Disease.
If you’re managing heart conditions with multiple medications, the cardiovascular benefits of psyllium (cholesterol reduction, blood pressure support) make it worth the timing effort. Use psyllium husk tablets for convenience if your schedule is complex – they’re easier to time consistently.
Inflammatory Bowel Disease.
IBD patients often benefit from psyllium but may take numerous medications, including immunosuppressants and anti-inflammatories. Work closely with your gastroenterologist on timing, as some IBD medications have very specific absorption requirements.
Practical Tips for Managing Psyllium with Medications.
Create a Medication-Psyllium Schedule.
Write out your daily medication times, then highlight safe windows for psyllium. Keep this schedule visible until it becomes automatic. Most people find consistency within 2 weeks.
Use Phone Reminders.
Set alarms for both medications and psyllium. Title them clearly: “Morning Meds,” “Psyllium Safe Window,” “Evening Meds.” This removes guesswork.
Communicate with Your Pharmacist.
Your pharmacist can review your complete medication list and advise on specific timing concerns. They often catch interactions your doctor might miss.
Start Psyllium on Weekends.
Beginning psyllium when you have schedule flexibility lets you experiment with timing without work pressures. Once you find a rhythm, weekday implementation is easier.
Keep a Brief Log.
For the first two weeks, note medication times, psyllium times, and any symptoms or issues. This helps identify patterns and optimal timing for your situation.
Choose One Psyllium Format and Stick with It.
Consistency aids both habit formation and predictable medication interactions. Whether you choose psyllium husk tablets, psyllium husk capsules, or powder, maintain that format for at least a month before evaluating results.

Common Myths about Psyllium and Medications.
Myth 1: “I Can’t Take Psyllium If I’m on Medications”.
False. You absolutely can take psyllium with medications – you just need appropriate timing separation. Millions of people successfully use both daily.
Myth 2: “Psyllium Husk Tablets Don’t Interact Like Powder Does”.
Not true. All psyllium forms create the same gel that affects absorption. Tablets simply dissolve more slowly, potentially extending the interference window.
Myth 3: “Taking Psyllium with Meals Prevents Medication Problems”.
Actually, taking psyllium with meals can increase interaction risks if you take medications with meals. The safest approach is to keep psyllium and medications in separate meal windows.
Myth 4: “More Water Prevents Absorption Issues”.
Water helps psyllium work properly and prevents constipation, but it doesn’t eliminate medication binding. Time separation is what matters for absorption.
Quality and Purity Impact on Medication Interactions.
Higher-quality psyllium creates more predictable interactions. Low-grade psyllium with contaminants or inconsistent fiber content makes timing calculations unreliable.
Pakistani psyllium, particularly from Sindh province, offers exceptional purity – often 95-99%. This consistency means you get the same fiber dose every time, making medication timing more reliable. At Malik Psyllium, our processing ensures consistent husk quality, whether in powder, capsule, or tablet form.
Lower-quality products may contain:
- Variable fiber content (affecting gel formation).
- Seed particles (unpredictable absorption effects).
- Processing residues (additional interaction risks).
- Inconsistent particle size (erratic dissolution).
For medication users, quality isn’t a luxury – it’s essential for predictable, safe use.

When to Consult Your Healthcare Provider.
Always discuss psyllium addition with your healthcare provider if you:
- Take more than 3 prescription medications.
- Use medications with narrow therapeutic windows.
- Have chronic conditions requiring precise medication control.
- Take immunosuppressants or chemotherapy drugs.
- Experience unexplained medication side effects.
- Notice symptoms suggesting inadequate medication absorption.
Your doctor can order blood level testing for critical medications to ensure therapeutic ranges are maintained despite psyllium use.
Monitoring Effectiveness after Adding Psyllium.
Signs Your Medications Are Still Working.
- Chronic conditions remain controlled.
- No return of symptoms that medications manage.
- Blood tests show therapeutic drug levels.
- Blood pressure, blood sugar, or other metrics stay stable.
Signs of Possible Absorption Issues.
- Return of symptoms previously controlled by medication.
- Unexplained worsening of managed conditions.
- Blood tests showing subtherapeutic drug levels.
- Increased symptom variability.
If you notice these signs after starting psyllium, increase the separation time between psyllium and medications, or consult your healthcare provider about timing adjustments.
Integrating Psyllium Successfully into Your Medication Routine.
The key to successfully managing psyllium husk and medication absorption is treating fiber supplementation as seriously as you treat your medications. Here’s my final integration strategy:
Week 1:
Establish baseline. Take medications as prescribed without adding psyllium. Note your usual medication times.
Week 2:
Map safe windows. Identify gaps of 3-4 hours where psyllium fits. Choose your preferred format (powder, psyllium husk capsules, or psyllium husk tablets).
Week 3:
Start psyllium at half dose in your identified safe window. Monitor medication effectiveness.
Week 4:
Increase to full psyllium dose if no issues arise. Continue monitoring.
Week 5+:
Maintain consistent timing. Adjust as needed based on lifestyle changes.
This gradual approach lets you identify any issues early while building sustainable habits that serve both your medication regimen and digestive health goals.
How does psyllium husk affect medication absorption?
Psyllium forms a viscous gel that can bind medications, slow gastric emptying, and coat intestinal walls, reducing drug absorption. Proper timing separation (2-4 hours) prevents interference while allowing you to enjoy psyllium’s benefits safely.
Should I take psyllium husk tablets or capsules with medications?
Both psyllium husk tablets and psyllium husk capsules require separation from medications – tablets need 3-4 hours, capsules need 2-3 hours. Powder offers the shortest interference window. Choose based on your medication schedule complexity and convenience needs.
What’s the best time to take psyllium if I’m on medications?
Take psyllium during the longest gap between critical medications – typically mid-morning or early evening. Ensure at least 2-3 hours from any medication, and 4 hours from thyroid or heart medications.
Can I take psyllium husk capsules with my morning medications?
No, separate them by at least 2-3 hours. Take morning medications first, then wait until mid-morning for psyllium husk capsules. This ensures full medication absorption before fiber creates interference.
Do psyllium husk tablets interfere with medications more than powder?
Psyllium husk tablets dissolve more slowly, potentially extending the interference window to 3-4 hours. Powder acts faster with a shorter interference period. Both require separation, but tablets need slightly more time.
Which medications need the most separation from psyllium husk?
Thyroid medications, diabetes drugs, heart medications (digoxin), blood thinners, and seizure medications require 3-4 hours of separation. Antibiotics and antidepressants need 2-3 hours. Consult your pharmacist about your specific medications.
Can psyllium reduce the effectiveness of my prescriptions?
Yes, if taken too close together. Psyllium husk and medication absorption conflicts occur when timing is inadequate. Proper separation (2-4 hours) prevents this issue completely while maintaining both medication effectiveness and psyllium benefits.
Are psyllium husk tablets better than capsules for medication users?
Neither is inherently better – it depends on your schedule. Psyllium husk tablets offer precise dosing but need more separation time. Psyllium husk capsules are easier to swallow but require multiple pills. Powder offers the most timing control.
Conclusion.
Managing psyllium husk and medication absorption doesn’t have to be complicated. With proper timing separation – 2-4 hours depending on your specific medications – you can safely enjoy psyllium’s remarkable digestive, cardiovascular, and metabolic benefits without compromising your treatment effectiveness.
The format you choose matters too. Psyllium husk tablets offer convenience and precise dosing but require longer separation times. Psyllium husk capsules provide easy swallowing with moderate timing needs. Traditional powder gives you the most control over timing and remains the most economical option. All three work effectively when used correctly.
Remember that quality significantly impacts consistency and reliability. Pakistani psyllium, particularly premium-grade products like Malik Psyllium, provides the purity and consistency that make medication timing more predictable and trustworthy. When you know exactly what you’re getting in every dose, managing interactions becomes straightforward.
Start slowly, establish clear timing protocols, communicate with your healthcare providers, and monitor your results. Most people successfully integrate psyllium into their medication routines within 2-3 weeks, enjoying improved digestive health alongside effective disease management. The key is respecting both your medications and psyllium’s powerful properties – give each the space and timing it needs to work optimally, and both will serve your health goals exceptionally well.
Malik Shabbir
Featured Blogs

Isabgol Ke Fayde – Psyllium Husk Ke Poori Science-Based Rahnumayi – 2026
Isabgol ke fayde jaanna aaj ke daur mein zyada zaroori

Isabgol Benefits in Hindi | Psyllium Husk Ke Fayde, Sahi Upyog Aur Savdhaniyan – 2026
Agar aap isabgol benefits in hindi mein samajhna chahte hain,
